Content Analysis of Patient Safety Incident Reports for Older Adult Patient Transfers, Handovers and Discharges: Do they Serve Organisations, Staff or Patients?
Scott, Jason, Dawson, Pamela, Heavey, Emily, De Brún, Aoife, Buttery, Andy, Waring, Justin and Flynn, Darren (2021) Content Analysis of Patient Safety Incident Reports for Older Adult Patient Transfers, Handovers and Discharges: Do they Serve Organisations, Staff or Patients? Journal of Patient Safety, 17 (8). ISSN 1549-8417
|
Text
Content analysis of patient safety_Dawson.pdf - Accepted Version Restricted to Registered users only Download (259kB) | Request a copy |
||
|
Text
Tables and Appendices for Content Analysis_Dawson.pdf - Supplemental Material Download (385kB) | Preview |
|
![[img]](https://marjon.repository.guildhe.ac.uk/17499/3.hassmallThumbnailVersion/Figure%201%20-%20300dpi.png)
|
Image
Figure 1 - 300dpi.png - Supplemental Material Download (208kB) | Preview |
|
![[img]](https://marjon.repository.guildhe.ac.uk/17499/4.hassmallThumbnailVersion/Figure%202%20-%20300dpi.png)
|
Image
Figure 2 - 300dpi.png - Supplemental Material Download (37kB) | Preview |
Abstract
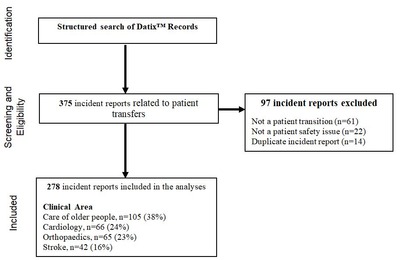
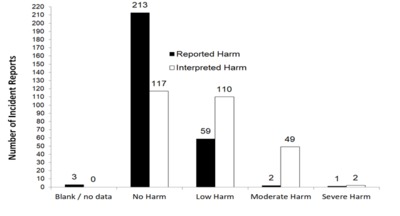
Objectives: Analyse content of incident reports during patient transitions in the context of care of older people, cardiology, orthopaedics and stroke. Methods: A structured search strategy identified incident reports involving patient transitions (March 2014 – August 2014, January 2015 – June 2015) within two NHS Trusts (in upper and lower quartiles of incident reports/100 admissions) in care of older people, cardiology, orthopaedics and stroke. Content analysis identified: incident classifications; active failures; latent conditions; patient/relative involvement; and evidence of individual or organisational learning. Reported harm was interpreted with reference to National Reporting and Learning System criteria. Results: A total 278 incident reports were analysed. Fourteen incident classifications were identified, with pressure ulcers the modal category (n=101; 36%) followed by falls (n=32, 12%), medication (n=31, 11%) and documentation (n=29, 10%). Half (n=139; 50%) of incident reports related to inter-unit/department/team transfers. Latent conditions were explicit in 33 (12%) reports; most frequently, these related to inadequate resources/staff and concomitant time pressures (n=13). Patient/family involvement was explicit in 61 (22%) reports. Patient well-being was explicit in 24 (9%) reports. Individual and organisational learning was evident in 3% and 7% of reports respectively. Reported harm was significantly lower than coder-interpreted harm (p<0.0001). Conclusions: Incident report quality was sub-optimal for individual and organisational learning. Under-reporting level of harm suggests reporter bias, which requires reducing as much as practicable. System-level interventions are warranted to encourage use of staff reflective skills, emphasising joint ownership of incidents. Co-producing incident reports with other clinicians involved in the transition and patients/relatives could optimise organisational learning.
| Item Type: | Article |
|---|---|
| Depositing User: | Ms Kerry Kellaway |
| Date Deposited: | 17 Oct 2019 16:53 |
| Last Modified: | 04 Jun 2025 14:10 |
| URI: | https://marjon.repository.guildhe.ac.uk/id/eprint/17499 |
| Related URLs: |
https://journal ... dent.99235.aspx
(Publisher URL)
|
Actions (login required)
 |
Edit Item |